Latest news about Bitcoin and all cryptocurrencies. Your daily crypto news habit.
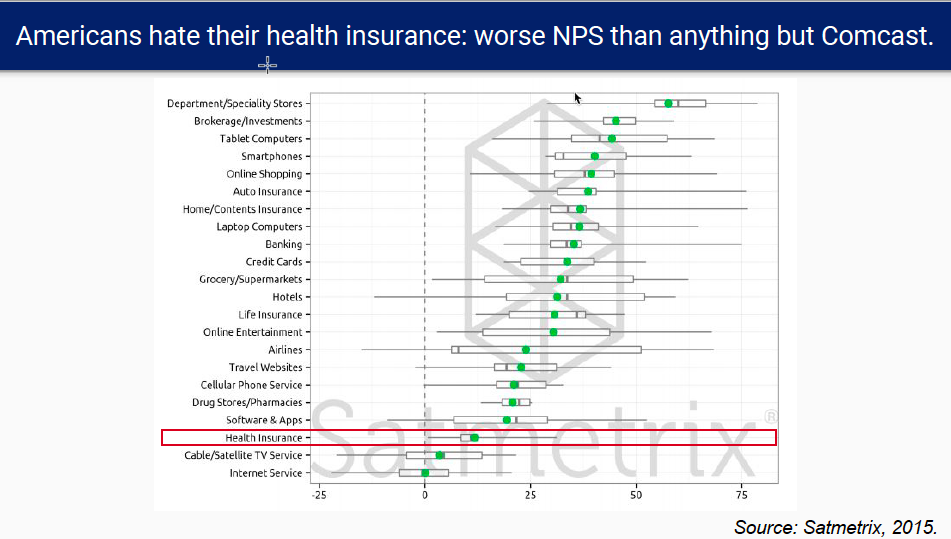
Americans hate their health insurance more than everything but Comcast. Literally: the industry gets a lower net promoter score than any other except TV and internet services.
Net promoter score (NPS) by U.S. industry
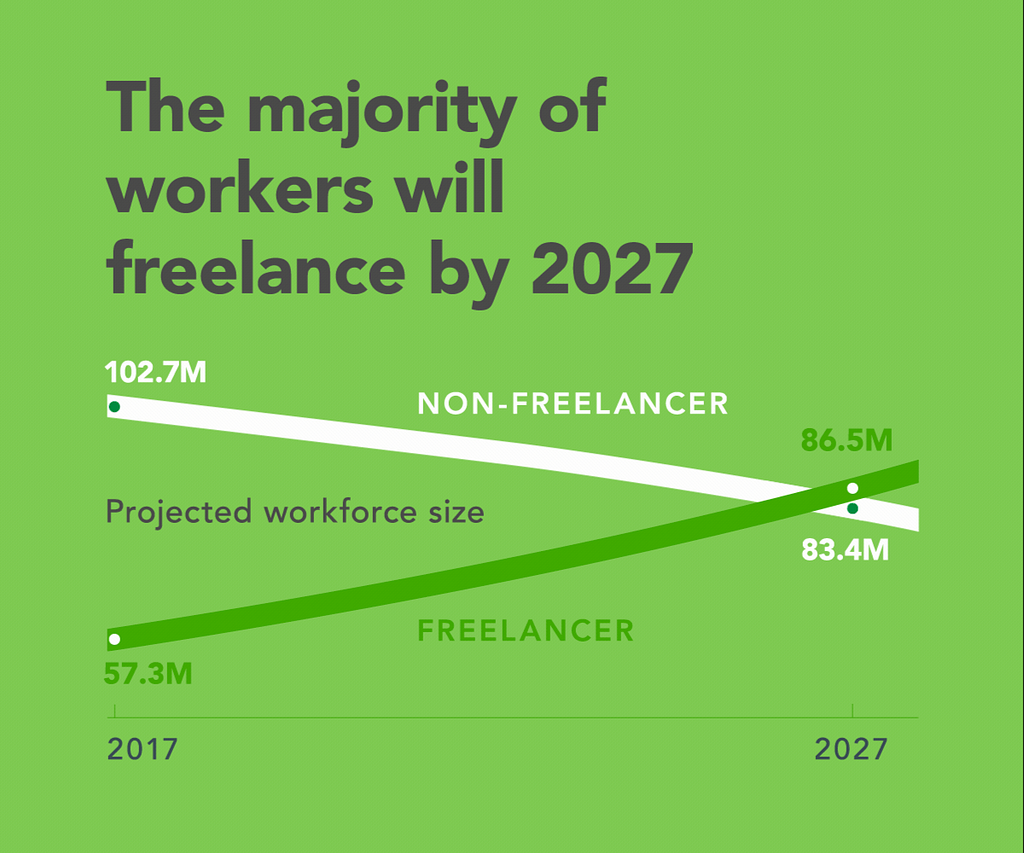
We hate our health insurance because it’s too expensive. Rising premiums, deductibles, copays, and coinsurance have formed a vacuum lock on household budgets. Many of America’s 57MM freelancers are hit hardest of all, since they buy their own insurance rather than getting it via work or the government. Most of us at Decent have worked as freelancers, so we know this problem firsthand — and according to the 2017 Freelancing in America survey, US freelancers are expected to outnumber non-freelancers by 2027.
Today, freelancers are buying overpriced insurance on the ACA exchanges, paying for short term or indemnity plans that don’t cover serious illness, or not buying insurance at all and putting their lives and families at risk. Some are hacking together their own alternatives: enrollment in non-insurance solutions such as religious health sharing ministries, which don’t guarantee coverage and require members to sign a statement of faith, rose 74% from 2014 to 2016.
It’s no wonder people are struggling. 43% of purchasers in the individual market don’t qualify for subsidies on their monthly premiums — premiums that have increased by 123% for individuals and by 174% for families since 2013.
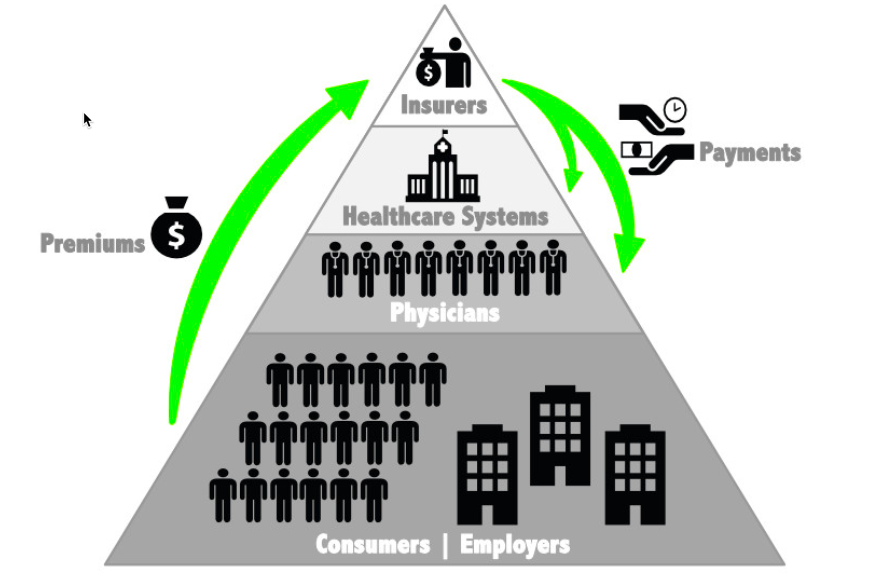
Over the same period, the CEO of UnitedHealthcare has received more than $270MM in compensation. Insurers sit at the top of the healthcare food chain because they control the money, collecting premiums from consumers and employers and paying health systems and providers: a massive rent-taking middleman with more power than any other stakeholder over the data, design, and delivery of healthcare.
The healthcare food chain, Vince Salvo 2018
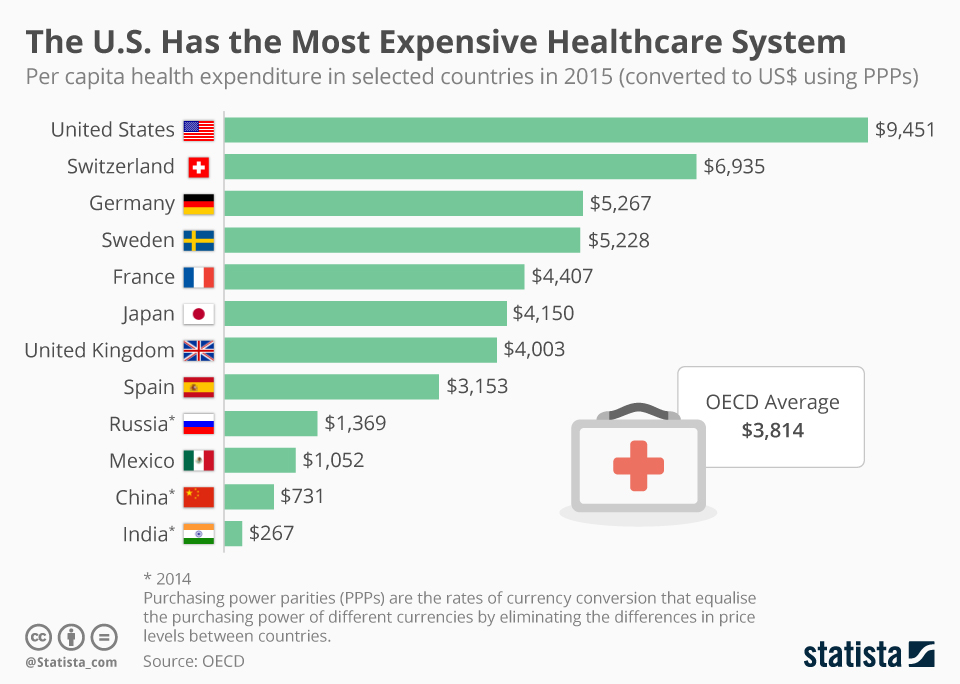
People in the United States pay more for healthcare, but get less.
U.S. healthcare is the country’s largest private-sector industry, with over $3.5 trillion ($3,500,000,000,000) dollars spent every year — about 75% of it via health insurance. With 13% of its workforce employed by the industry, the United States spends more on healthcare per capita than any other country — over $10,000 per person — but often places dead last in global health rankings.
Per Capita Healthcare Spend by Country, OECD 2015
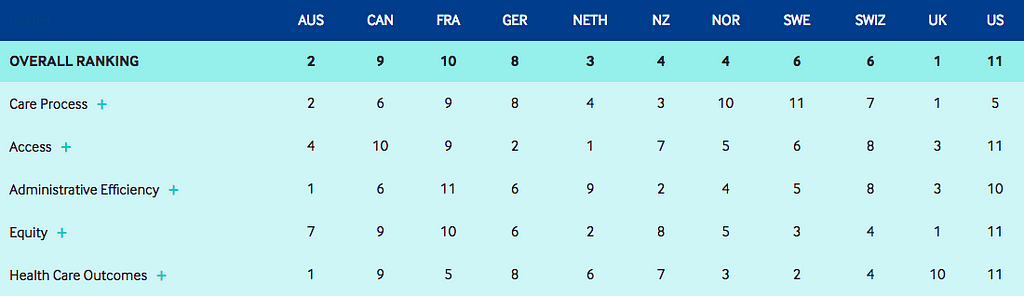
Health Care System Rankings,The Commonwealth Fund 2017
Clearly the United States is not paying for quality. Its citizens have the shortest life expectancy among the 20 most industrialized nations: a baby girl born in the U.S. in 2015 could expect to live for about 81 ½ years — 5 years less than a baby girl born in Japan. America isn’t paying for quantity either: costs continued to rise in 2016 as utilization of services declined or stayed flat. Americans are paying the highest prices, and we are not getting our money’s worth. An open-heart surgery that costs $150,000 in the U.S. can be performed at an institution in India with equal or better clinical outcomes for $2,000. According to the Kaiser Family Foundation, the U.S. has the highest rates among comparable countries of deaths preventable by health care; years lost to disability and premature death; hospital admissions for preventable diseases; medical, medication, and lab errors; obesity; and mortality rates from respiratory disease. U.S. adults are less likely than those in comparable countries to have fast access to doctors and nurses when they need it, and are more likely to go to the emergency room for conditions that could be treated by a regular doctor.
How did we get here?
Healthcare and ethics were bound together from the start. The earliest written references to healthcare appeared around 1754 BC in Hammurabi’s Code: the laws governing Mesopotamia, the world’s first known civilized society. Hammurabi specified a sliding scale of what doctors should be paid — ten shekels of silver to care for a lord, five shekels for a poor man, or two shekels for a slave — along with clear penalties for failure: “If a physician performs a major operation on a lord … and causes his death … they shall cut off his hand.”
Western medicine has its roots in ancient Greece. Asclepius, the Greek god of medicine and healing, carried a serpent-entwined rod still recognized as the symbol of medicine today. Greeks introduced the concepts of diagnosis and prognosis. Hippocrates, often called the “Father of Medicine”, established medicine as a separate discipline from theology, arguing that disease was the product of environmental factors, diet, and living habits rather than a punishment inflicted by the gods. He penned the original Hippocratic Oath still sworn by modern physicians, encoding ethics into healthcare around 400 BC: “I will use treatment to help the sick according to my ability and judgment, but never with a view to injury and wrong-doing. … I will keep pure and holy both my life and my art.”
America’s first health insurance plan was born from equally pure intentions in 1929, when Dallas educator Justin Ford Kimball observed that teachers couldn’t afford to get sick: “They were unable to face the costs of paying hospital bills. At the same time, Baylor [University Hospital, where Kimball was an administrator] was in desperate need of money … It owed more than $1.5 million.”
Kimball developed a plan to let Baylor’s patients, who were mostly teachers, prepay 50 cents per month to cover up to 3 weeks in the hospital per year, starting with week 2 of any stay. Week 1 was billed at $5 per day — the original co-pay to discourage unnecessary care. His model assumed all hospitals were nonprofits, and aimed to make sure hospitals got paid what they spent on patient care — meaning from the start, the plan paid what the hospitals charged. It was an immediate hit, with 75% of Dallas teachers signing up.
With a new industry established, profiteering wasn’t far behind. Patients at nearby Methodist Hospital complained that the new plan was only for Baylor patients. Kimball offered to expand it, but Methodist administrators partnered with a commercial insurer instead, who added a quarter (50%!) to the monthly premium as his commission. Kimball began to market his plan in local newspapers and then via hospitals, which valued the recurring revenue, under the imprint of a blue cross.
With the support of hospital finance departments, the business that would become Blue Cross Blue Shield expanded rapidly to become the largest health insurance company in America, covering 1 of 3 Americans in all 50 states. In 2016 it spent over $25MM on lobbying, more than any other company in America — and just ahead of the American Hospital Association, the Pharmaceutical Research and Manufacturers of America, and the American Medical Association. The bonds between healthcare and ethics have been frayed, if not severed: large business interests are doing all they can to maximize profit, not health. By writing the rules of the game, these interests make it more difficult for small emerging innovators to try new models and gain a meaningful footprint.
Healthcare costs driven by greed and waste are bankrupting the U.S. middle class.
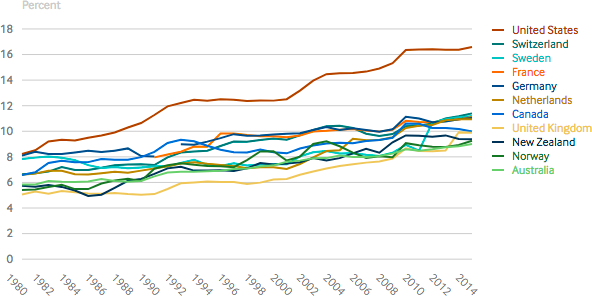
U.S. healthcare costs have steadily risen as a percentage of Gross Domestic Product (GDP) since 1980, to over 18%: twice the average of 9% spent by other developed nations.
Health Care Spending as a Percentage of GDP, CMS 2018
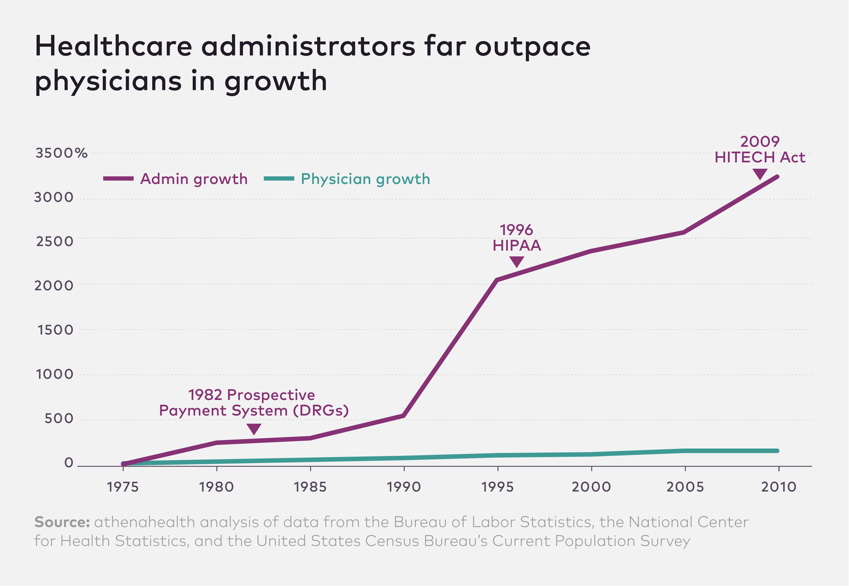
A major driver is administrative waste: experts estimate that over 30% of healthcare spend, or over 1 trillion dollars every year, is waste — and the number of middlemen and administrators has skyrocketed vs. physician growth since 1970 (Exhibit 6).
Growth of Physicians and Administrators, Bureau of Labor 2010
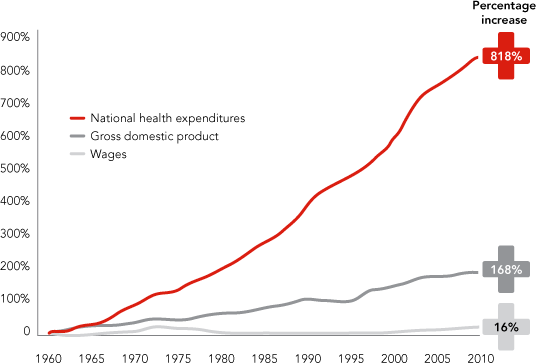
Rising healthcare costs have fueled a multi-decade economic depression of the American middle class. Economic gains have been passed on disproportionately to the wealthy: growth in U.S. healthcare costs has outpaced growth in wages since 1960 by a staggering tally of 818% vs. 16%. Healthcare costs are the country’s leading cause of bankruptcy. Almost 80% of Americans say they live paycheck to paycheck, and nearly half of Americans would need to borrow or sell something to come up with even $400 for an emergency expense — and 1 in 5 had experienced a unexpected medical expense in the last year, with an average cost of $2,782.
Health Care Spending Growth vs. GDP and Wages, McKinsey 2011
For decades healthcare costs including insurance have stopped poor and middle class Americans from getting ahead. And they’re only getting higher as baby boomers age, enter Medicare and are subsidized by younger generations. CMS expects healthcare spending to rise 5.5% annually from 2017 to 2026 and comprise 20% percent of GDP in 2026.
Meanwhile, 2017 is expected to mark the third straight year of decline in U.S. life expectancy, fueled primarily by the opioid epidemic killing millions of Americans with commercially available drugs — and matching a dubious streak only seen before from 1916 through 1918, a period that included the worst flu pandemic in history.
Many have suggested that healthcare defies the laws of business. In every other industry, innovation and market forces have worked in tandem to push down costs and improve quality over time. Something must be different about healthcare. But what?
Stay tuned. In Part 2, we’ll share the root cause and what Decent is doing to fix it.
Why is health insurance in America such a bad deal? (Part 1) was originally published in Hacker Noon on Medium, where people are continuing the conversation by highlighting and responding to this story.
Disclaimer
The views and opinions expressed in this article are solely those of the authors and do not reflect the views of Bitcoin Insider. Every investment and trading move involves risk - this is especially true for cryptocurrencies given their volatility. We strongly advise our readers to conduct their own research when making a decision.